Due to the dryness and fragility of the annulus fibrosus, herniated discs are more often present in age-related osteochondrosis. But this is only one of the risk factors. Others include:
- Because of being overweight, the waist bears a heavy burden.
- Muscles are weak.
- Genetic.
- A sedentary lifestyle, as a result, the vertebral structure is constantly under pressure.
- smokes.
- Great physical activity.
According to medical statistics, the incidence of this disease in men is several times that of women.
What are the most common causes of the disease:
- Injured from a road accident or fall.
- Lift heavy objects with incorrect load distribution.
- Scoliosis or lordosis, causing increased pressure in certain areas of the spine.
- Hip dysplasia.
- Chronic diseases, including spinal tuberculosis, tumors, and syphilis.
- Metabolic disorders (hereditary and acquired).
All these factors can cause the cartilage and bones of the spine to wear and weaken. This is also the main cause of herniated disc.
Stage of disease
Without proper treatment, the disease will progress and the condition of the damaged intervertebral disc will worsen. The development of the disease has four stages:
- Prolapse. The intervertebral disc has moved a lot, no more than two millimeters. The nucleus pulposus does not protrude from the vertebral body.
- Lumbar spine protrusion. The edge of the intervertebral disc extends beyond the vertebral body by a distance of 1. 5 mm, but no displacement of the nucleus is observed.
- extrusion. The nucleus pulposus protrudes beyond the vertebral body.
- isolate. The nucleus actually falls off and hangs on the vertebrae in the form of water droplets. At this stage, there is a risk of rupture of the annulus fibrosus and leakage of fluid secretions.
In the first stage of the disease, a person hardly worries about anything. Sometimes low back pain will occur, but it will pass quickly. As the disease progresses, health conditions are getting worse and symptoms become more painful and alarming. If the diagnosis is not timely and the treatment is not started, the consequences may be: leg paralysis and severe nervous system disorders.
What are the manifestations of lumbosacral hernia?
Intervertebral hernia can manifest as the following symptoms:
- Pain in the waist.
- Pain during walking, radiating to the thigh area.
- Numbness in the surface area of the feet, fingers, calves, and thighs.
- Feeling heavy in the legs.
- The stiffness of the movement.
In order not to delay medical treatment, it is necessary to carefully analyze the symptoms of the disease. They can be divided into three groups.
Pain syndrome
Pain of lumbosacral hernia is a major symptom. Even in the first stage, there is pain in the area of the damaged intervertebral disc, especially after the injury. They can increase or decrease, and then reappear. More commonly, the sacral area will not even be painful, but will be painful, especially when physically exhausted or sedentary. If a person lie down on the healthy side and bend their legs, the pain will completely subside. This situation can last for several months.

It is easy to get rid of the problem by seeking medical help through timely treatment. Say goodbye to bad habits and do the physical therapy exercises recommended by your doctor.
Every day, the affected area will increase and the condition of the intervertebral disc tissue will deteriorate. The second transition to disease is marked by increased pain. It is now not only in the sacrum area, but also covers the entire lower back, radiating to the neck area, every spine muscle, buttocks, thighs, legs, feet and toes. Discomfort is manifested as physical activity, even trivial-coughing or sneezing.
Vertebral Syndrome
The worsening of the pain in the second stage is accompanied by continuous spasms of the back muscles. This makes the patient more uncomfortable. He cannot move freely, straighten his back, and stretch. The gait of such a person becomes uncertain, he always leans to the opposite side of the patient and is listless.
Due to impaired motor coordination, the quality of human life declines. He was unable to complete the tasks at work well, and it became unrealistic to take active rest due to constant pain.
Nerve root syndrome
If the doctor does not pay attention to the hernia, the progressive disease can cause compression of the spinal cord roots, causing them to die, and it is almost impossible for blood to enter the tissues of the damaged intervertebral disc. Features of the severe stage of the disease:
- The leg muscles are weakened. The patient cannot squat, stretch, or jump. Even climbing stairs is difficult for him.
- Numbness in the affected area and surrounding areas. The skin became numb and pale, with goose bumps and tingling sensations. Patients complain of excessive sweating in the affected area and legs, or, conversely, excessive dryness of the skin.
- Low back pain. The patient suffers from low back pain, which is severe and aggravated with any exercise. If left untreated, it can cause damage to the hip and knee joints.
- The painful leg is noticeably thinner, resulting in an asymmetrical posture.
- Destruction of pelvic organs. Urinary and gynecological diseases are aggravated, libido disappears, diarrhea, and urinary incontinence are possible.
In severe cases of spinal cord hernia, there is a risk of paralysis, disability and even death.
Pathological diagnosis
If a person has severe back pain, he needs to make an appointment with a neurologist. He will be checked by medical tests:
- Identify reflexes from the tendons of the lower limbs.
- Leg raise test.
- Measure the sensitivity of the entire surface of the legs, thighs, buttocks, abdomen, and back to heat or cold, pain, and vibration.
The doctor will then refer the patient for an MRI or CT scan of the lumbar spine. With the help of tomography technology, a three-dimensional image of the affected area will be obtained. It can be used to determine the location and size of the hernia, and the stage of the disease.
If there is a risk of spinal cord injury, additional electromyography, neuroimaging, and contrast myelography are prescribed. With the help of these studies, doctors will determine whether emergency surgical intervention is needed.
Herniated Disc Treatment
The treatment of intervertebral disc herniation is divided into conservative treatment and surgical treatment. The choice of technology depends on the development stage of the disease, the existence of accompanying diseases and contraindications.
Conservative treatment
The main purpose of the treatment process is to relieve pain and relieve the patient's condition.
What medicine can the doctor prescribe:
- Medicine to relieve pain and inflammation. In case of deterioration-in the form of injection. When the acute pain is relieved (usually three to four days are enough), oral medications with similar effects are prescribed.
- Novocaine blocker with corticosteroids. A similar method can relieve pain for two weeks at a time. Usually, a series of blockages are performed by injection into different parts of the damaged intervertebral disc.
- Centrally acting muscle relaxant. They reduce muscle activity by relieving pain and cramps.
- Vitamin-mineral complex, emphasizing group B elements. They relax muscles slightly, help tissue regeneration and the conduction of nerve impulses.
After the pain syndrome is relieved, the intake of drugs is reduced. The treatment of the disease is due to physical therapy and physical therapy.
The physical therapy treatment method is also selected according to the patient's condition. this might be:
- Treat with heat or electric shock.
- Electrophoresis with anti-inflammatory drugs.
- Acupuncture and acupoint massage.
- Spa.
- Hydro massage.
Normal massage is only allowed if there is no pain syndrome. A more effective physical therapy is a post-isometric relaxation manipulative therapy.
The doctor strongly advises smokers to quit smoking.
Nutrition adjustment is also very important, especially for overweight patients. Fats, savoury dishes, sweets and alcohol must be excluded from the menu. A diet that contains a lot of vegetables and fermented dairy products will help the body better tolerate treatment and reduce back weight.
operation treatment
Conservative treatment usually lasts about two months. If it does not give the expected results, decide to change the treatment strategy or perform surgery. The latter is used to treat severe pain, loss of leg sensitivity, and pelvic organ dysfunction. According to the complexity of the situation, the operation is carried out in the following way:
- Endoscopic method. Make three micro incisions in the affected area. A camera was introduced into it and used to broadcast to the monitor. With the other two, a micro instrument is used to remove the hernia protrusions.
- Through the method of percutaneous discectomy. The damaged nucleus is removed by puncturing the intervertebral disc and replaced with artificial material.
- Reconstructed by laser. It uses a special needle in the form of puncture, without dissecting tissue. Laser radiation heats the structure of the intervertebral disc and stimulates cell regeneration and relieves pain.
In difficult situations, intradiscal prosthesis is possible-replacing injured organs with implants.

After complex surgical intervention, rehabilitation will be required. The surgeon must wear a corset and cannot take a sitting position for about three months. The further rehabilitation period involves the practice of therapeutic gymnastics and physical therapy.
Preventive techniques
Like any other disease, a herniated disc is easier to prevent than cure. What you need to do to keep your intervertebral disc healthy:
- If your work is load-related, or you are a professional athlete, please calculate the load accurately.
- The correct weight (the index should not exceed 30).
- Choose a good mattress to sleep in the correct posture (best lying on your back).
- Engage in gentle sports, swimming, and fitness.
- Add exercises to the morning exercises to strengthen the muscles of the spine.
- Quit smoking.
- Eat well.
If following these rules becomes a habit, then it is possible to get a spinal hernia due to an accident.
Intervertebral disc herniation is dangerous, with serious consequences, and the treatment time for advanced cases is very long. To avoid surgery and complications, if you feel back pain, you should see a neurologist.
Osteochondrosis
The word osteochondrosis itself comes from two words: bone-bone and cartilage-cartilage. Simply put, it is cartilage ossification. Although this explanation is fundamentally wrong. Some people’s delusions go further. They believe that osteochondrosis is the accumulation of salt in the joints. In addition, it is said that a large amount of food is table salt.
Onset
In reality, everything has happened something different. And it's harder. And salt, if it plays any role in the pathogenesis of osteochondrosis, it is very indirect. Osteochondrosis is based on malnutrition and degradation of articular cartilage. This is not an independent disease, but a pathological process that can be noticed almost anywhere with connective cartilage tissue.
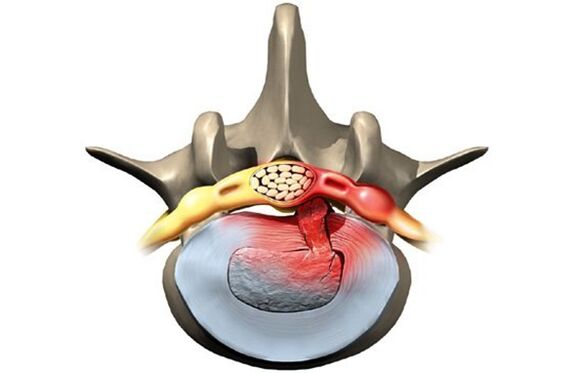
Nevertheless, osteochondrosis affects the spine in most cases. why is that? The fact is that there is a kind of spacer between the vertebrae-intervertebral disc (intervertebral). The physiological role of these intervertebral discs is to cushion and protect the vertebral body from premature wear caused by mechanical stress. The intervertebral disc consists of an internal fluid nucleus, surrounded by an annulus fibrosis and an upper and lower endplates.
The intervertebral disc is subjected to tremendous mechanical stress, causing permanent damage to its structure at the cellular level. In humans, these processes are too obvious-this is the price we pay for walking upright. In order to prevent the disk from being completely "erased", it must be regenerated continuously, that is, restored. The balance of the injury-regeneration process determines the normal structure of the intervertebral disc. Another strange detail is that the blood and nutrient supply to the intervertebral disc is not carried out through the overgrowth of blood vessels in childhood, but through the diffusion of the bone tissue of the vertebral body. Again, pay for the ability to walk on two legs, not all fours.
Therefore, in terms of anatomy and physiology, the intervertebral disc is easily injured. Any negative process in the body can lead to an imbalance of injury and regeneration, and lead to malnutrition and degeneration of the intervertebral disc. An optical disc with a defective structure can no longer withstand proper mechanical stress. Under excessive pressure from the overlying vertebrae, the intervertebral discs shift in different directions, usually to the sides and back. This process is called herniated disc.
The bone tissues of the vertebrae that have lost their cartilage lining are also subject to mechanical abrasion. Due to the continuous trauma to the anterior surface of the vertebral body, pathological bone growth-osteophytes was formed. Spondylopathy develops. Due to the degeneration and displacement of the intervertebral disc, the intervertebral space shrinks, the spinal canal narrows, and the spinal nerve roots are violated. Intervertebral foramen.
reason
The causes or causes of osteochondrosis are diverse. They can all be local, that is, caused by the pathology of the spine itself and general diseases at the biological level. Any pathology that leads to the destruction of the spine structure or metabolic disorders can be considered as the cause of osteochondrosis. In this regard, there are:
- Changes in the structure of the spine (scoliosis, pathological lordosis or kyphosis)
- Other defects of the musculoskeletal system-flat feet, narrow shoulder straps, pelvic abnormalities
- Spinal injury
- Weak immunity
- Metabolic disorders-osteoporosis, obesity, diabetes, thyroid disease
- Cardiovascular diseases-atherosclerosis, hypertension
- Digestive system diseases that cause insufficient absorption of nutrients in the gastrointestinal tract
- Genetic.
It should be noted that the above pathological conditions do not necessarily cause osteochondrosis. This requires constant exposure to certain predisposing factors-hypothermia, malnutrition, a sedentary lifestyle, or, conversely, excessive physical exertion.
symptom
Osteochondrosis itself is an asymptomatic process. At the same time, the signs of intervertebral disc degeneration are also diverse. How could this be? In fact, the clinical manifestations of osteochondrosis are based on its complications-intervertebral disc herniation, spondylopathy, sciatica, spinal stenosis.
In addition, according to the main location of the process in the cervical, thoracic, or lumbosacral spine, clinical manifestations vary greatly. The last part is most often affected because it is the most physical activity undertaken by the lower back. Signs of lumbosacral osteochondrosis:
- Pain (low back pain, low back pain, sciatica)
- Limited movement of lower back and lower limbs (intermittent claudication)
- Here, sensory disorders of the paresthesia type-numbness, burning, peristalsis
- Pathological tension of psoas muscle
- In the absence of treatment, pelvic organ dysfunction.
Compared with the lumbosacral region, the frequency of observation of cervical osteochondrosis is slightly lower. However, this pathology is also very common. In addition to the typical signs of pain (neck pain), upper limb sensitivity and decreased movement, cervical osteochondrosis due to impaired blood supply to the brain has its own characteristics. These characteristics are manifested in:
- Insomnia
- Headache, dizziness
- Periodic nausea
- General weakness and fatigue
- Blood pressure fluctuations
- Occasionally toothache
- Behavioral reactions such as tearing and irritability.
The chest area with osteochondrosis is relatively unaffected. In this case, the patient is someone who is forced to sit in an uncomfortable fixed position due to occupation-student, schoolchild, programmer, office worker. In this case, the symptoms of osteochondrosis are as follows:
- Chest pain and paresthesias
- Difficulty breathing
- The feeling of heartbeat
- Limitation of thoracic spine movement.
diagnosis
In summary, osteochondrosis is a chameleon disease. Because of the similar physical signs, it is easy to be confused with cerebrovascular accidents, hypertension, myocardial infarction, angina pectoris, neurosis, etc. This is why, in order to make a correct diagnosis, a comprehensive and complex diagnosis is needed to correctly determine the symptoms and treatment of osteochondrosis.
This diagnosis, in addition to traditional inquiries and clarification of patient complaints, should also include medical examinations and special research methods. These methods include spinal X-rays and visceral ultrasound. Recently, computers and magnetic resonance imaging have been successfully used to diagnose osteochondrosis.
treat
Treatment strategies for osteochondrosis include the use of:
- drug
- massage
- Physiotherapy procedures
- Physical therapy (exercise therapy)
- Manual therapy
- acupuncture.
Drugs used to treat osteochondrosis are mainly aimed at relieving pain and eliminating the inflammatory process of nerve roots. For this, use NSAID drugs. In various combinations, these drugs are widely used in the treatment of osteochondrosis in the form of ointments, injections, and tablets. It should not be forgotten that these drugs have a negative effect on the liver, stomach and intestines. By doing so, they can aggravate the metabolic disorder of osteochondrosis. They used local anesthetics to relieve the pain caused by the blockade. It is true that the effect of these funds is short-lived and will never affect the entire course of osteochondrosis.
With the help of drugs such as chondroprotective agents, immune stimulants and vitamins containing minerals, it can improve the local and body-level metabolic processes. Chondrprotectants are used in tablets, ointments and ampoules. In fortifiers, vitamin C and B groups are used together with minerals. In this regard, calcium preparations are most preferred. In fact, contrary to some false claims, the basis of osteochondrosis is not an excess of calcium, but only a lack of calcium.
After successfully alleviating the deterioration, show physical therapy, massage and exercise therapy. Calcium electrophoresis, hydrocortisone ultrasonic electrophoresis, amplipulse, paraffin therapy are used as physical procedures. All these measures aim to eliminate pain and inflammation of nerve roots, ligaments and muscles. Perform osteochondrosis massage according to generally accepted methods. Select the massage area according to the location of osteochondrosis. The expansion of the range of motion is achieved with the help of exercise therapy. At the beginning, during the deterioration phase, there is almost no dynamic load. The patient is always in the best posture. At this time, it is best to wear fixation devices-waist girdle, Shants neck brace. As the deterioration disappears, the amount and duration of exercise during exercise therapy increases.
Recently, in the treatment of osteochondrosis, non-traditional treatment methods have been accepted-acupuncture, manual therapy, and osteopathy. Acupuncture is an effect on special biologically active spots located on the spine, auricles, hands and feet. Through manual treatment, the normal position of the vertebrae and intervertebral discs is restored by the manual movements of the hands of the expert. During osteopathy, the structural integrity of the musculoskeletal system is ensured by specific techniques. In the absence of conservative measures to treat osteochondrosis, persistent pain, and complications, surgery is required. The pathologically displaced disc was removed. Currently, for this purpose, a microdiscectomy-endoscopic removal of displaced discs is performed.



































